Its major difference from the closed tray technique is that the impression coping case stays fixed tight in impression paste. That is why there arises a need to unscrew the fixing screw before we take the impression out of the mouth and, consequently, to use a monophasic impression material. Let us review this technique step by step.
First, the impression coping should be chosen in accordance with the height, so that an impression tray with the paste cab be taken through between the fixing screw and the tooth-antagonists 3.2-4C. Then, make a hole in the impression tray above the fixing screw that makes it possible to pull this screw out (actually, because of this hole this method got the name of “open tray impression”).
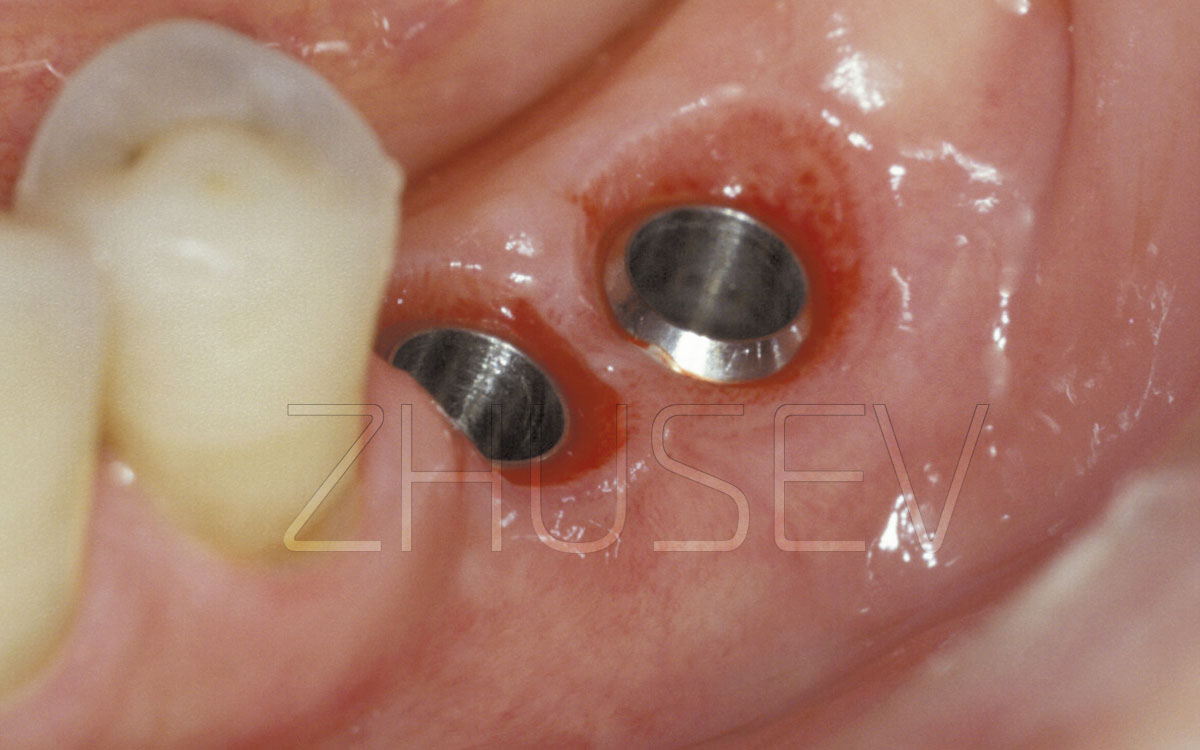
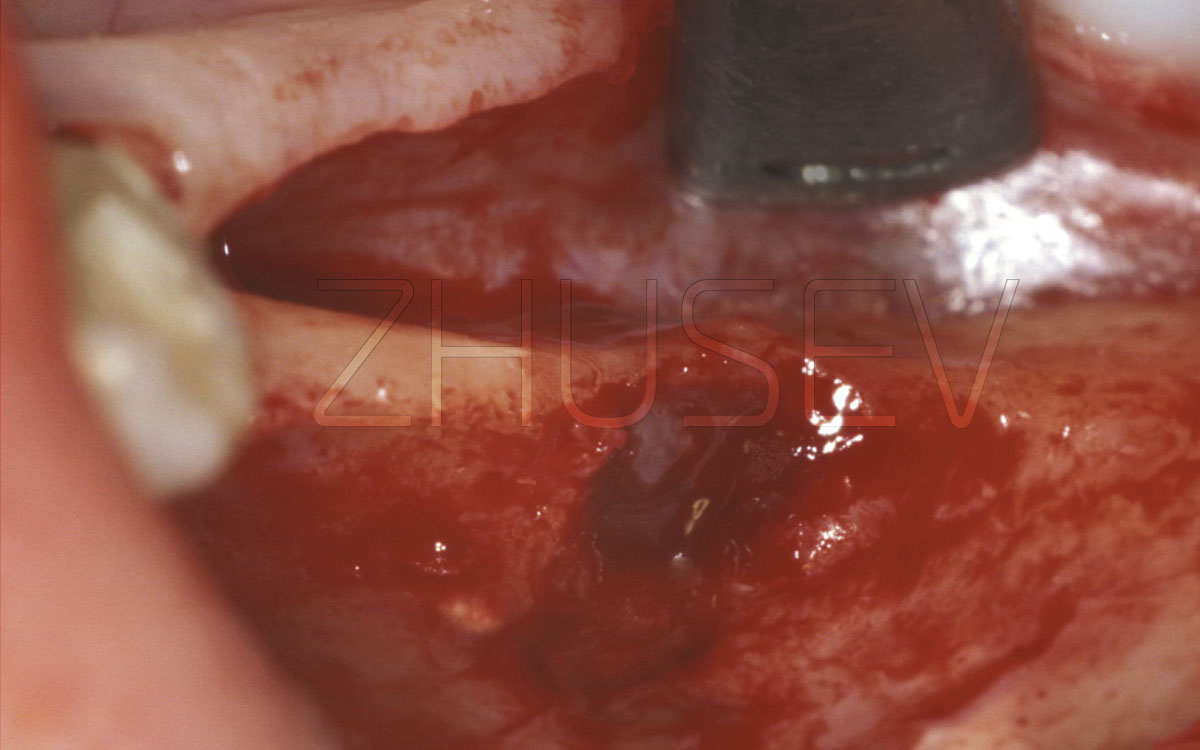
Insert the impression coping into the implant and tighten the fixing screw. Put the impression material (such as Impregnum) on the tray and take into the mouth. After the mass hardens, first unscrew the fixing screw 3.2-4D and only then take the tray from the mouth (of course, never take this tray into the mouth again and don’t re-use the corrective compound).
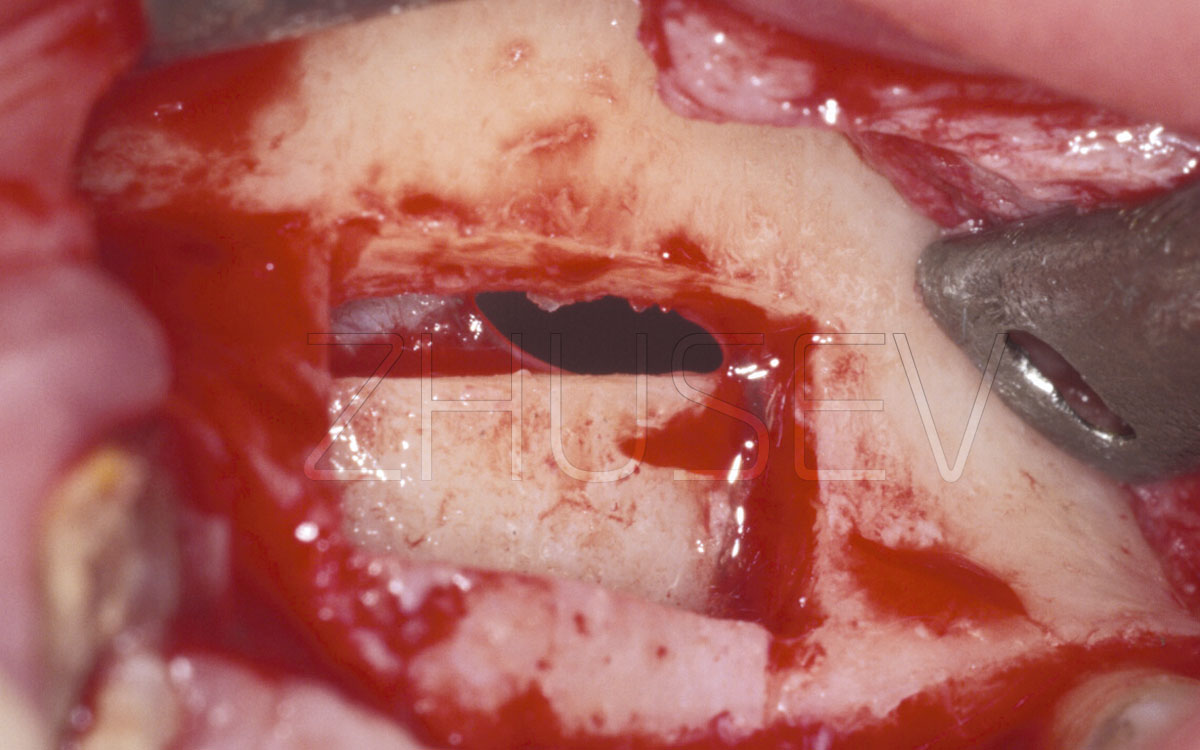
In this case, the impression coping should stay fixed tightly in the impression paste. Then the dental technician attaches an implant replica directly to it (with the impression coping still being placed in the impression paste). Next, in the same way, as with the previous technique, we fill the part of the implant replica with a gingival mask and cast a base of the model of die stone.
Generally speaking, if you work accurately and carefully, using either technique will not influence the quality of transferring your implant to another position. Try to take a few impressions using different techniques, and analyse the results. Ideally, you should master both these techniques in practice equally well. And in time, you will be able to choose the right method for a specific purpose.
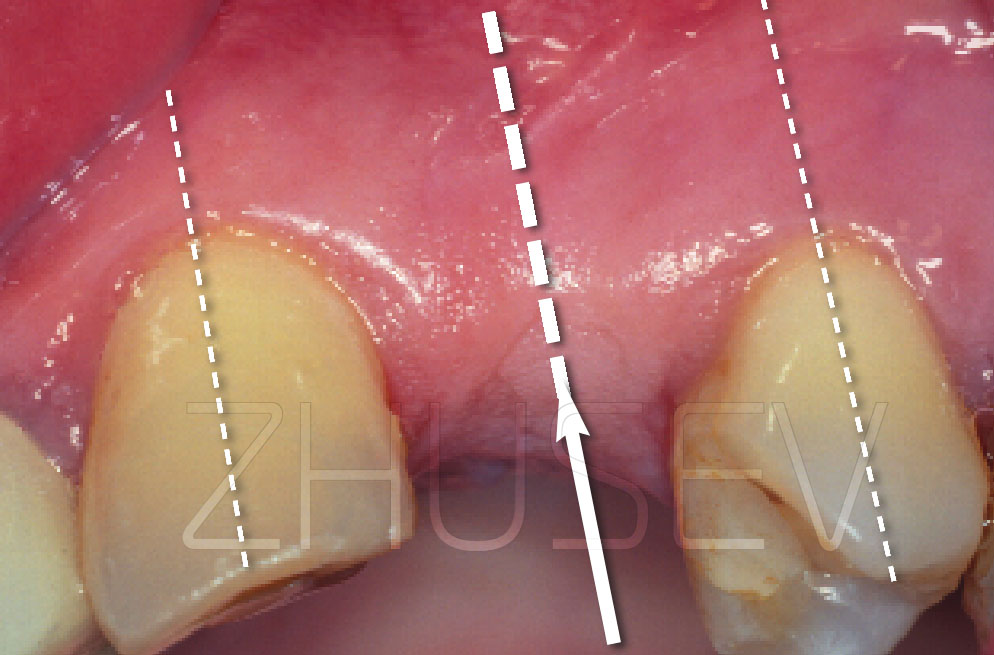
But let us come back to the dental laboratory and see what happens then. As a result of the above procedures, the dental technician makes a gypsum master cast with a metal implant replica, fixed in accordance with the implant’s position (and its place) in the mouth. And then with consideration of required inclination of the implant, the interdental height, etc., we select the type of the future crown’s bearing part, called a suprastructure (a supporting head or an abutment). All implant manufacturers produce a wide range of suprastructures of different heights, diameters, and angulations. It will be better if the suprastructure is chosen by a dental technician in the laboratory, but not an orthopedic surgeon in his office. On the gypsum model, all positions and inter-relations can be seen better. This way, the selection procedure will be more effective.
After the suprastructure is selected, the dental technician makes a model of the wax composition of the future crown and then casts it of metal. Before putting the ceramic paste 3.2-4M, it makes sense to try on the completed metal framework in the mouth, to make sure that it squeezes no soft tissues around the implant.