The most common problem of the early post-operative period is hematomas, which can differ as to their volume and site.
Unfortunately, there is no sure way to avoid formation of hematomas. To prevent them, you can use the safe and proven method of local application of cold and (or) a pressure bandage. To accelerate resolution of the hematoma apply Troxevasin or Actovegin.
Sometimes 3-7 days after the surgery there appears an oedema and tension under one of the flaps lifted during the surgery, which then develops into a purulent process. All clinical signs resemble those of dental periostitis. In 9 out of 10 cases, the process begins in the lower jaw. Thinking it over I’ve come to a conclusion that it must be caused by the following factors: the surgeon is traditionally situated on the right side of the chair and the nurse on the left side, during the whole operation she holds the dental aspirator in one hand and the retractor hook in the other.
why under the flap, where there is no active aspiration, accumulate fragments of bone chips, epithelium, etc. With a certain bacterial and immune background it creates favourable environment for pus formation. And if your nurse (assistant) is right-handed and stands behind the patient, she usually holds the aspirator in her right hand and the retractor hook in her left hand. That’s why in the third quadrant the aspirator is situated under the lingual flap and in the fourth quadrant under the buccal flap.
As a result, the inflammatory process, vice versa, develops under the buccal flap in the third quadrant and under the lingual flap in the fourth quadrant. That’s why before suturing the wound, carefully flush the area under both flaps with saline solution with simultaneous aspiration!
Here, we should remember, that the prophylaxis of infectious inflammatory processes in the post-operative wound, which can bring all your efforts to failure, is still one of the major tasks. It is known that prevention of complications is much easier and safer than treatment of a process that has already developed. The traditional means for this purpose is the use of antimicrobial drugs and antiseptics. But we also should never forget such prevention techniques as: shortening the surgery time, hospital-provided infection control, observance of the asepsis principles, equipping the operating room with sterilizing lamps with forced and natural air circulation, etc.
Also you should take into account the preparation technique of the implant bed for installation (the use of a sharp tool with an optimum way of heat and chips removal, an adequate cooling technique, following the routine of preparation, etc.). It is known that more than 30% of antibiotics proscriptions is made for prophylaxis. When planned properly, antibiotic prophylaxis can decrease the complication rate manifold. One of the major factors that influence wound infection is the microbial content level. Depending on this, all implantological procedures can be subdivided into 4 groups:
While planning the antibiotic prophylaxis you should take into account the following rules:
Certainly, the choice of specific drugs and their dosage are very individual. But in my practice, the medicine that showed a nice result is Amoxiclav 625 mg (the first intake: two pills are taken 2 hours before the operation plus one pill before going to bed. Then 1 pill should be taken twice a day (for prophylaxis the course should go on for 3 days, at the risk of possible complications – 5-7 days). A good result was given by the treatment with Avelox 0,4: 1 pill during 5 days. In the oral cavity, as a rule, there might be combinations of different unicellular organisms. That’s why in the postoperative period you can recommend the patient cleaning teeth with Metrogyl Denta tooth ointment, which should be put on a tooth-brush instead of toothpaste. After cleaning teeth don’t rinse your mouth too intensively!
Besides, it will be good to additionally assign some non-steroidal anti-inflammatory drugs (Ibuprofen, Хefocam, etc.). With patients who have an expressed postsurgical pain condition, nice results are provided by Indomethacin (aka Metindol Retard 75 мг) which should be taken once a day during 3-5 post-operative days. This medicine is one of the most active nonsteroidal anti-inflammatory drugs with a well-defined analgesic effect.
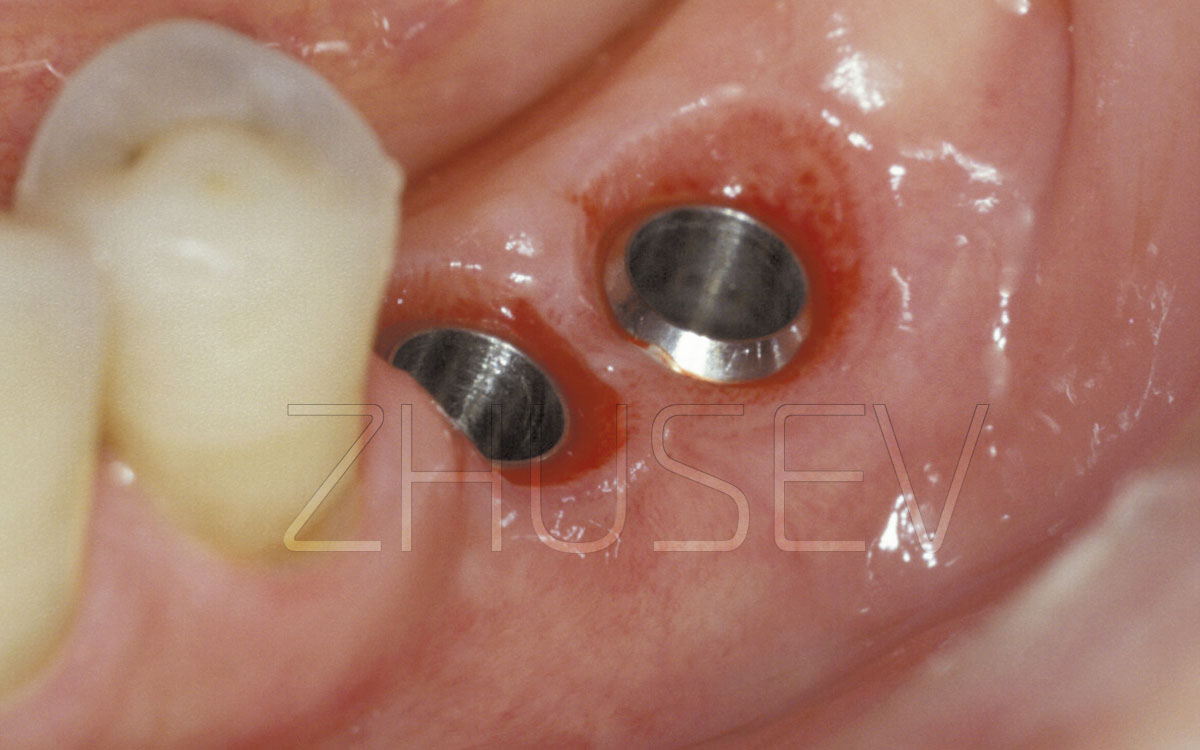
Removable, temporary and immediate dentures, mounted immediately above the surgical area, can cause large problems. In the case of mounting a temporary denture, supported on the adjacent teeth, try to provide just a minimal area for irrigation in such a way that the denture wouldn’t compress the mucosa in the places above the installed implants. With a removable denture, try to ensure that the denture’s base pressure on the implantation area will be minimal, via grinding its plastic material edges.
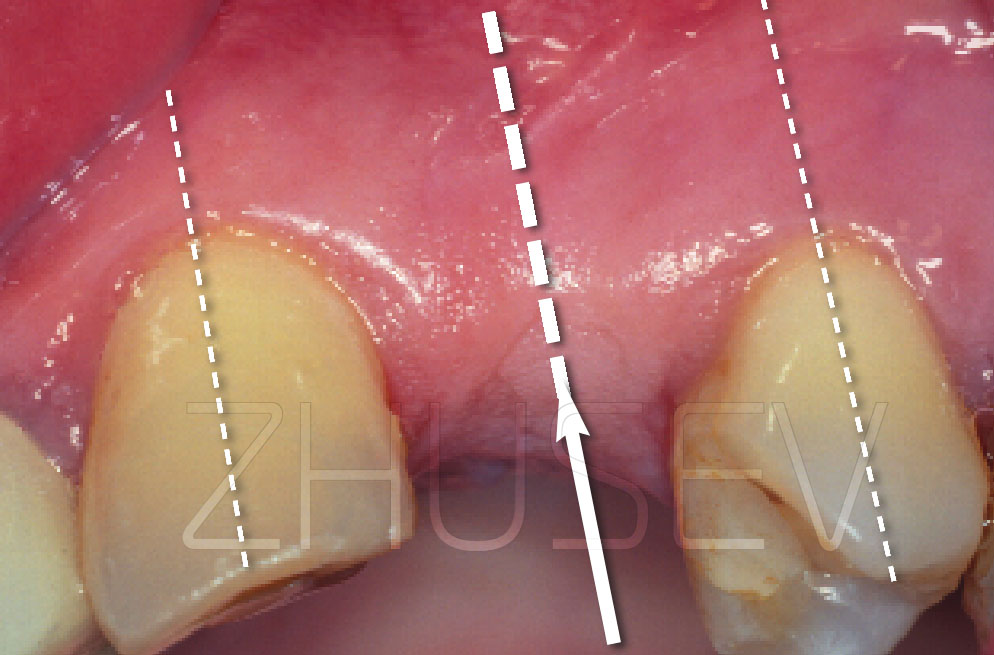
Pay much attention to the condition of the teeth, located in the proximity of the surgery area. In case of the slightest doubt about their condition, endodontic treatment should be provided before the surgery. Making a reference X-ray is also necessary.
Odontogenic and radicular cysts pose a major hazard, especially when the implant is installed nearby. The surgery procedure itself can provoke activation of these masses growth. If in these teeth performance of root apex resection is planned, a retrograde filling procedure should be done with the use of composite material. Never use amalgamation for this purpose.
Besides, never forget that titanium, implants in the presence of some electrolyte (saliva) and metals (crowns, fillings, the dentures fragments) can show different electrical potentials, which can not only cause rapid formation of bacterial plaque, but can also cause galvanic corrosion.
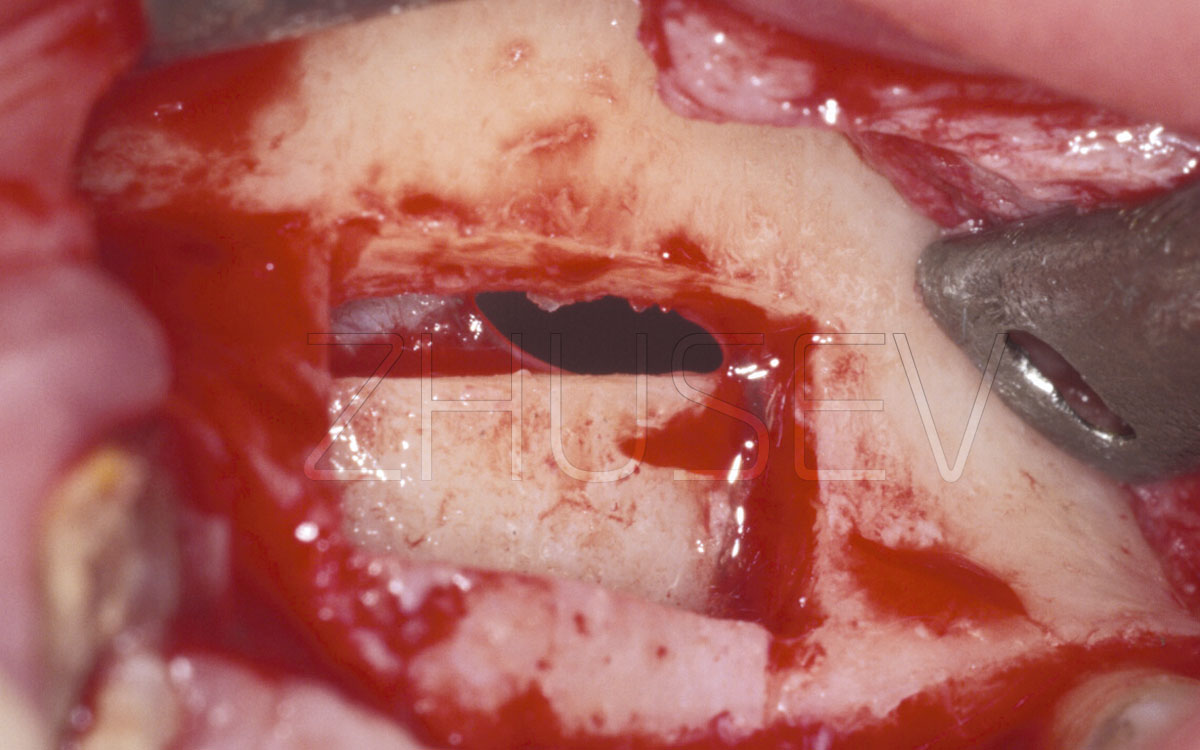
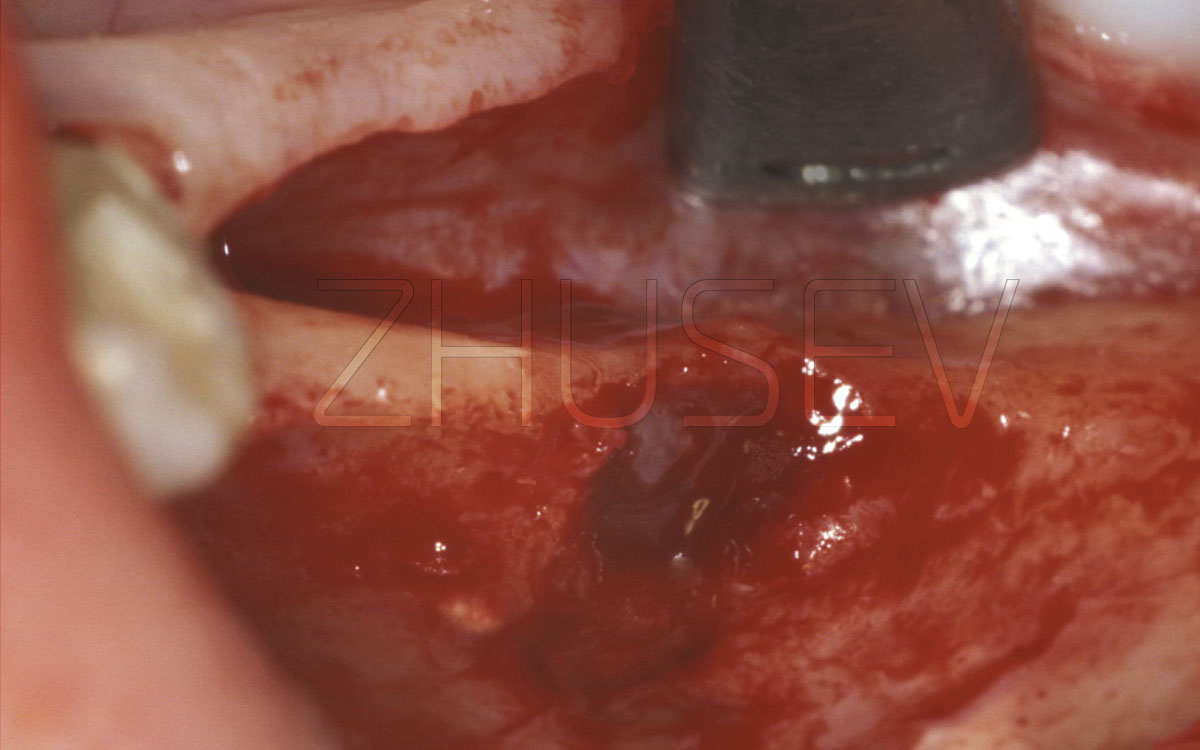
Look at the clinical case, which is presented on this page. The electrical potential that developed between amalgam and a titanium implant caused migration of the filling material elements and, as a result, loss of the implant.
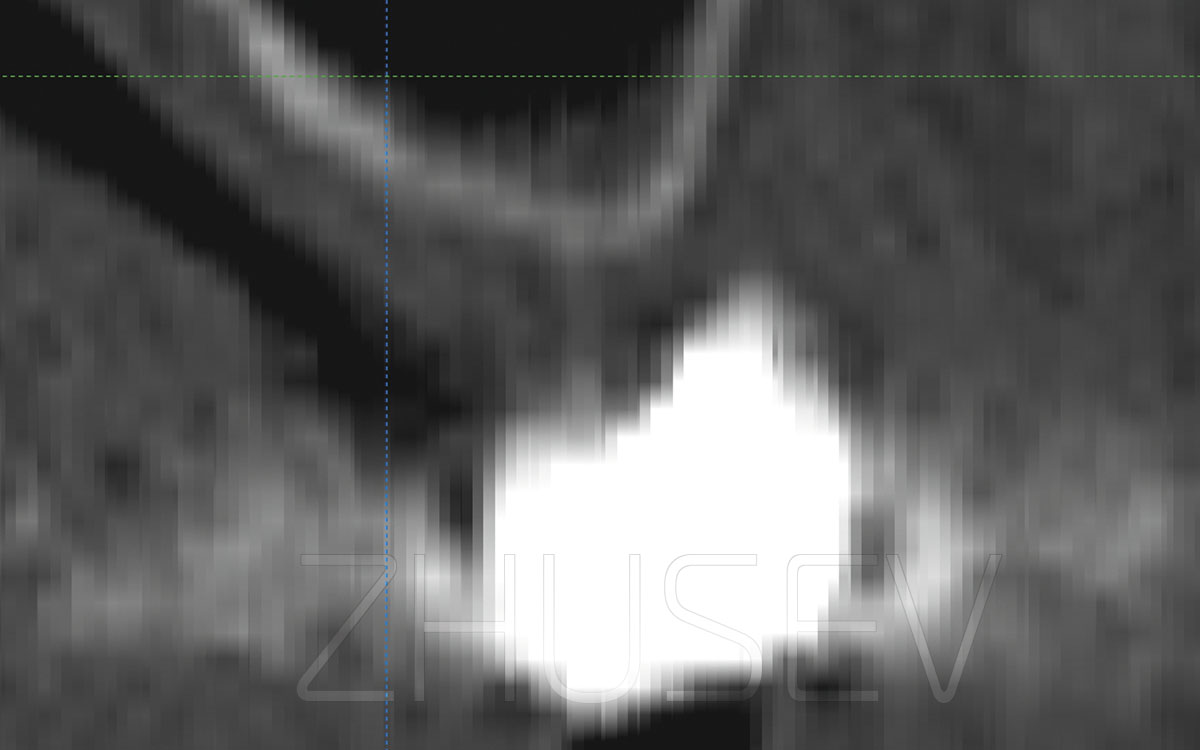
Of course we all know that conventional X-ray images (both periapical and orthopantomographical) nearly always contain projection distortions. And very often, these distortions are non-linear and non-proportional, which makes their correct interpretation difficult.
It happened many times when I had to face situations, when an implant that seemed to be ideally inserted (based on X-ray results) turned to be disintegrated and could be easily extracted with the use of hands only. At the same time, the implants with unfavourable X-ray results showed the absolute stability, caused no pain and no complaints from the patients.
In dental implantology, in particular, you can hardly make a judgement based only on the basis of an X-ray image, or only on the basis of oral examination data. While doing this, both the procedures’ results should be taken into account together.